Managing type 2 diabetes with medication.
The pros and cons of type 2 diabetes medication and their effects on diabetes patients at high risk of cardiovascular disease.
This article provides a topline overview to help people with type 2 diabetes begin discussions with their doctors. It is not a comprehensive document and is not intended to replace the advice of a doctor or other healthcare professionals.
Diabetes medications use a range of approaches to bring your blood sugar under control by affecting how the body handles insulin and/or sugar.
All medicines can cause side effects in some people. If you do suffer from any, it’s worth talking to your doctor as there may be ways to manage the side effects, or there may be another medicine that could work better for you. Speak to your doctor to find out more.
People with type 2 diabetes should reassess their medications every 3–6 months. Are you on the right medication for you? Read on to find out more and be sure to discuss it with your doctor!
Metformin (biguanides) is the first medicine generally prescribed to people with type 2 diabetes who require medication in addition to diet and exercise to maintain their target blood sugar level. Metformin is the only medicine in the biguanide class and is taken orally as a tablet. In some cases, other or additional medicines may also be considered depending on factors such as your cardiovascular risk or kidney problems.
Metformin works by reducing the amount of sugar your liver releases into the blood and helps your body respond better to insulin.
Potential benefits of Metformin:
Potential risks of Metformin:
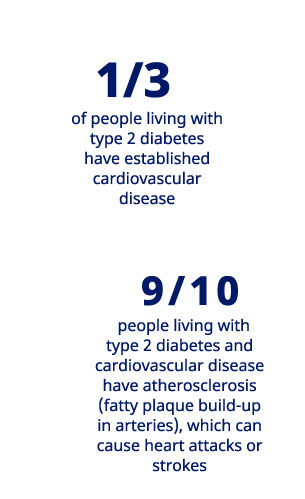
People with type 2 diabetes are 2-4 times more likely to have a heart attack or stroke compared to someone living without diabetes.
Learn how you can reduce the risk.
If you don’t need any extra protection for your heart or kidneys and your blood sugars are well-controlled, you may be able to stay on metformin alone. If your diabetes evolves and metformin is not enough to control your blood sugar alone, your doctor can recommend another treatment option.
A range of other treatment options is available, with a range of different combinations being possible. The medication map will be there to support you to navigate the treatments landscape!
Dipeptidyl peptidase-4 inhibitors (DPP-4is) are oral medicines that help increase the amount of insulin produced after eating and reduce the amount of sugar released by the liver when it’s not needed. They also slow down digestion.
Potential benefits of DPP-4is:
May help to control appetite
Potential risks of DPP-4is:
Common side effects include those of the gut, including diarrhoea and nausea, and flu-like symptoms
Thiazolidinediones are oral medicines that increase the body’s sensitivity to insulin and increase the amount of ‘good’ cholesterol in the blood.
Potential benefits of TZDs:
Potential risks of TZDs:
Sulfonylureas can be taken orally around a meal to simulate the production of insulin by the pancreas and increase the effectiveness of insulin in the body.
Potential benefits of SUs:
Long history of use and familiar effectiveness and side effect profile to doctors
Potential risks of SUs:
A diabetes doctor might prescribe glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and sodium-glucose cotransporter-2 inhibitor (SGLT-2is) to a range of different people living with type 2 diabetes for a range of reasons. However, these medicines may be particularly suited to people at risk of cardiovascular disease, heart failure or chronic kidney disease and are discussed in the next section.
GLP-1 RAs can be taken orally or given by a once-daily or once-weekly injection under the skin, depending on the medicine. GLP-1 RA medicines work in several ways: they slow down food leaving your stomach and help reduce the amount of sugar released from your liver. When your blood sugar gets high, GLP-1 RAs also increase the amount of insulin released by your pancreas.
Potential benefits of GLP-1 RAs:
Potential risks of GLP-1 RAs:
Side effects include those of the gut, including diarrhoea, nausea, and dizziness
SGLT-2is are oral medicines. These medications work to reduce blood sugars by preventing the kidneys from reabsorbing sugar back into the blood and therefore increasing the amount of sugar lost in the urine.
Potential benefits of SGLT-2is:
Potential risks of SGLT-2is:
HQ22DI00086