
Type 2 diabetes: your questions about insulin, answered
Are you about to start insulin treatment and want to learn more? Read about how insulin actually works in your body to help you feel more confident with your treatment.
If you’re living with type 2 diabetes, you might be wondering about insulin therapy. For many, insulin is the next step if initial treatments are not effective at keeping blood sugar levels under control1. If you’re feeling nervous about starting insulin injections, you’re not alone – and you probably have some questions2. Let’s explore some answers to common questions about the benefits of starting insulin, and important considerations for managing type 2 diabetes.
Remember, if you have any concerns around your diabetes management, it’s important to reach out to your healthcare professional to get the support you need.

In people with type 2 diabetes, the levels of sugar in the blood are too high – this is known as hyperglycaemia1.
Your body naturally produces insulin to keep your blood sugar levels within a healthy range. You could think of insulin as a key, that allows sugar to get out of the blood and into cells around parts of the body, such as the muscles1. However, if blood sugar levels stay high for too long, the insulin your body makes becomes less effective and your pancreas has to work overtime to produce more1.
For many, diet and exercise alone is enough to keep blood sugar levels under control and manage their type 2 diabetes1. However, as the disease progresses over time or if blood sugar levels stay high, it can be helpful to introduce medications to help you control your blood sugar levels1. Insulin is prescribed for people with type 2 diabetes to keep their blood sugar levels in a healthy range and prevent long term complications1.
Today there are many different methods for producing insulins able to mimic the hormonal response of someone who does not have diabetes.
In the early 1900s, insulin from pancreas cells was discovered to help treat type 1 diabetes, which led to the development of the first insulin treatment made from purified animal insulin3,4.
In the 1980s, insulin derived from animals was replaced with ‘human insulin’, which was made in a laboratory with DNA technology and is identical to the insulin produced by our bodies3.
Since the 1990s, different types of insulin called ‘insulin analogues’ were produced, which closely mimic the body’s natural pattern of released insulin4. Different types of insulin have different lengths of action; from helping with short-term control of blood sugar levels around meals (bolus insulin), to longer-term control of blood sugar levels (basal insulin)5. To this day, ongoing innovation in insulin therapies continues to improve the treatment of diabetes.
If you’ve been prescribed insulin therapy, the additional support it brings managing your blood sugar levels may help you keep the day-to-day symptoms of type 2 diabetes at bay.
When you eat and drink throughout the day, you’re taking in carbohydrates that cause your blood sugar to rise6. If it stays high, you can experience symptoms including excessive thirst, frequent urination and dry mouth1.
One of the advantages of insulin therapy is that is helps to control these day-to-day symptoms, as insulin works to lower the amount of sugar in your blood1. This can also help you feel more energetic in your daily life, with increased sugar stores within the rest of your body.
Another advantage of insulin therapy is it can help provide more control of your blood sugar levels around mealtimes, which can help to reduce the spikes in your blood sugar levels that you may experience after meals7.
If your blood sugar levels stays high for too long, you can develop more serious long-term complications, such as permanent damage to your nerves and eyes, as well as cardiovascular disease and chronic kidney disease8. Another important benefit of insulin therapy is that it can help prevent long-term complications by maintaining your blood sugar levels within a healthy range1.
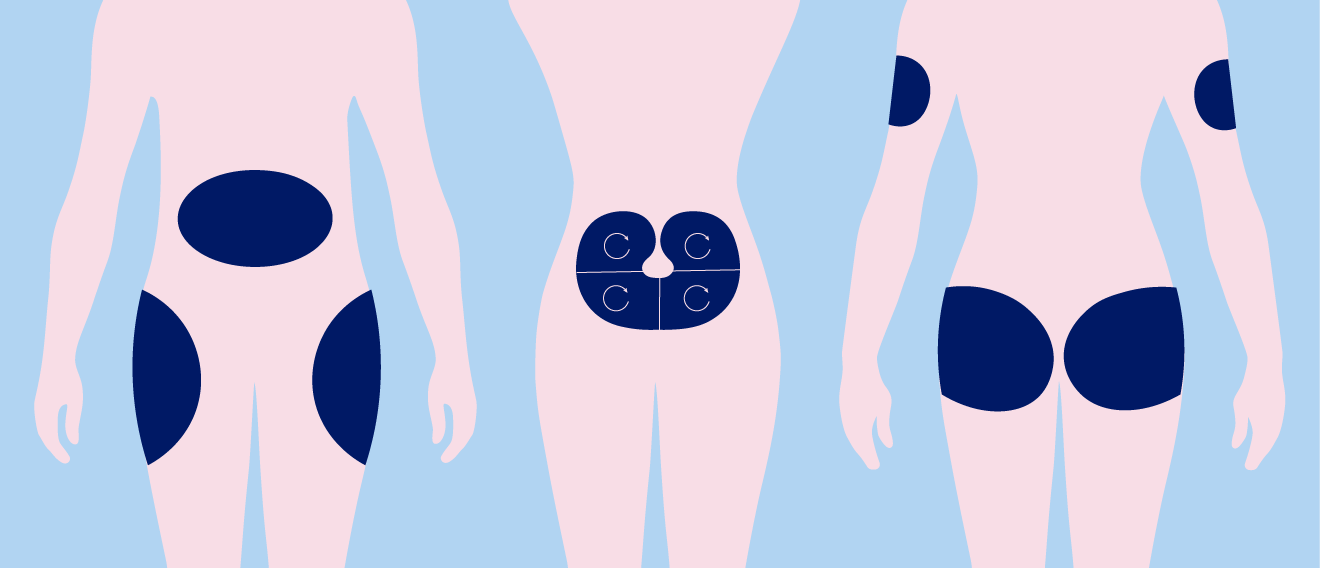
When you’re starting insulin therapy, it’s important to rotate injection sites to make sure you’re not accidentally impacting how much insulin you’re absorbing, or how fast it can get to work9.
If you’re injecting in the same location over and over, it may become inflamed, develop scar tissue or increase fat tissue under the skin, also called lipohypertrophy9. All of these factors can cause poor absorption, making your insulin therapy less effective at keeping your blood sugar levels within a healthy range9.
A healthcare professional can help you pull together a rotation routine that is right for you.
As a long-established, life-saving therapy option1, there aren’t ‘cons’ or disadvantages to insulin therapy when it is needed and prescribed by a healthcare professional – but of course there are things to be aware of when starting insulin therapy such as the adverse effects that you could experience when using insulin for your type 2 diabetes, and you may have some questions or concerns. We have covered some key questions below.
When starting insulin therapy, some people may experience weight gain10. This can be for a number of different reasons, including how much you take, your diet and the type of insulin you’re taking10. For example, as insulin is a growth hormone1, it can make you more hungry11. You may then eat more than you actually need and the excess sugar will be stored as fat11.
If weight gain is a concern for you personally, speak to your healthcare professional about managing it.
As it is a hormone, you can’t take insulin as a pill. Instead, it has to be injected. If you are worried about injecting or don’t like needles, you are not alone9,12!
It’s normal to feel anxious about injections at first. The most common needles you may be imagining are those used for vaccines, which typically use longer needles and are injected into the muscle. The good news is that for insulin, the needles used are much smaller and finer9,12. This means injecting insulin isn’t painful at all for many people.
Despite this, it’s okay to still be nervous! Following the right steps and techniques can help you work through it9,12. We’ve pulled together some tips for make injecting insulin more comfortable. Click here for more information on diabetes needle anxiety and top tips for injecting insulin.
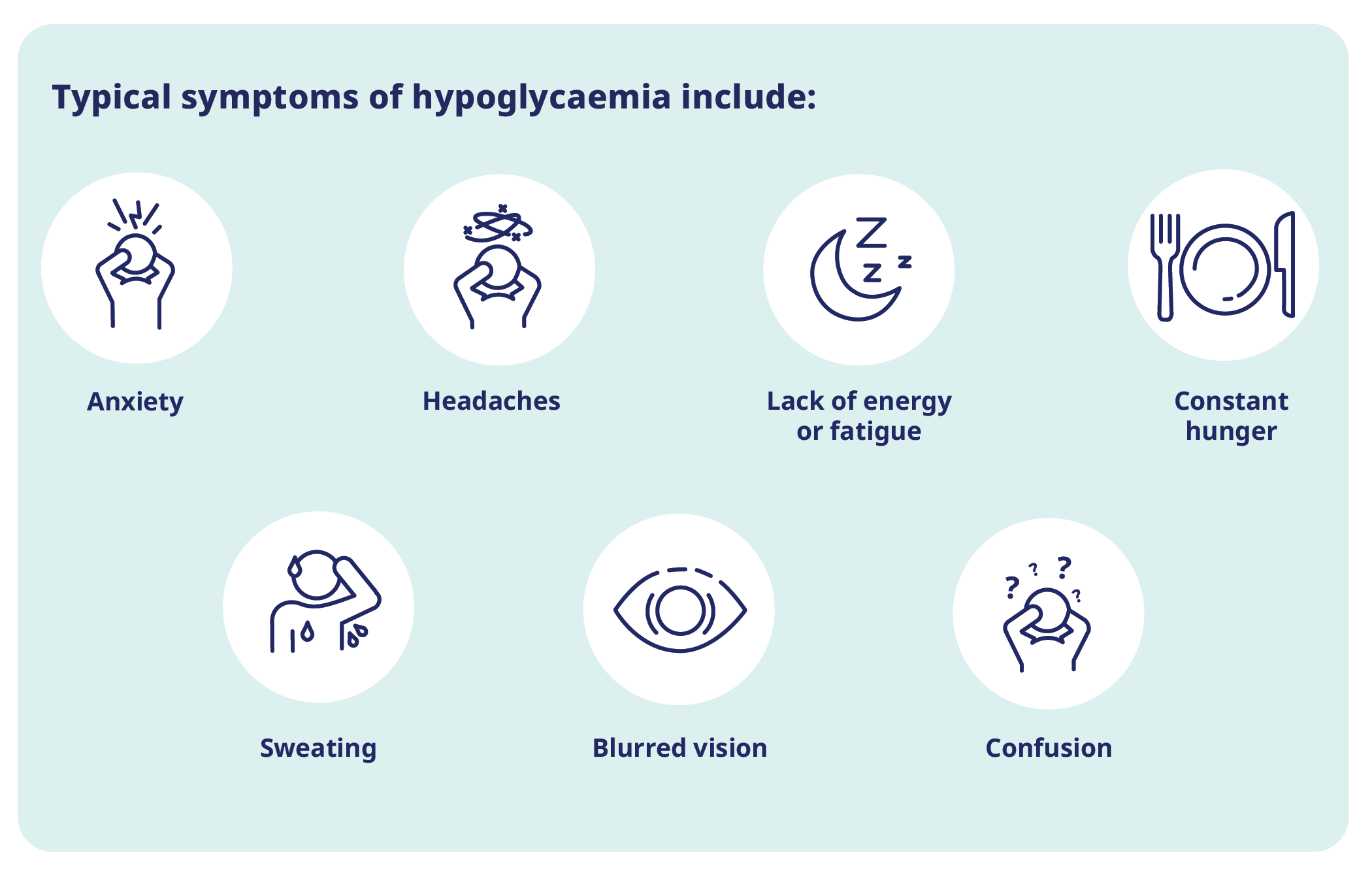
If you follow your treatment plan, well-managed insulin therapy poses minimal risk of complications9. However, taking insulin in improper dosages can be harmful as your blood sugar levels can drop too low and lead to hypoglycaemia1.
As too much insulin can lead to low blood sugar, the side effects to watch out for are the same as those for hypoglycaemia - starting off as hunger, anxiety, blurred vision, sweating and headaches13. They will be similar to what you experience if you skip meals.14 More severe side effects include mental confusion, loss of consciousness and seizures13.
If you suspect you’ve taken too much insulin or experience any of these side effects, seek medical help immediately.
No, insulin therapy aids with balancing your blood sugar levels1. When the right doses are taken, at the right time, your blood sugar levels should remain within a healthy range. That’s why it’s important to keep track of your blood sugar levels, stick to your prescribed insulin regime and know how to manage your symptoms to keep your blood sugar levels within a healthy range.
Starting insulin therapy might feel like a big change. You may be worried about injections, or even see it as a failure to manage your disease in other ways. These are normal reactions. But try to remember that it’s a positive change that will help you take control of your health and give your body the support it needs. With the right support and treatment, you can continue to live well with type 2 diabetes. If you have any remaining questions or concerns about insulin therapy, don’t hesitate to reach out to your healthcare professional.
Still have questions around starting insulin therapy for your type 2 diabetes? Read through our guide and take notes on questions you can ask your healthcare professional here.
HQ24DI00290

We spoke to real people living with type 2 diabetes to explore their experiences of starting and living with insulin therapy.
Explore the stories here.
1. International Diabetes Federation. IDF Diabetes Atlas Report 10th Edition 2021. Available at: http://www.diabetesatlas.org/ Last accessed: October 2024.
2. Peyrot M, Barnett AH, Meneghini LF, et al. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med. 2012;29:682-689.
3. Vecchio I, Tornali C, Bragazzi NL, et al. The Discovery of Insulin: An Important Milestone in the History of Medicine. Front Endocrinol (Lausanne). 2018;9:613.
4. Sims EK, Carr ALJ, Oram RA, et al. 100 years of insulin:
celebrating the past, present and future of diabetes therapy. Nat Med.
2021;27:1154-1164.
5. Donnor T, Sarkar S. Insulin- Pharmacology, Therapeutic Regimens
and Principles of Intensive Insulin Therapy. In: Feingold KR, Anawalt
B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya
K, Dungan K, Hofland J, et al., eds. Endotext. South Dartmouth (MA);
2000.
6. Holesh JE, Aslam S, Martin A. Physiology, Carbohydrates. In:
StatPearls. Treasure Island (FL); 2024.
7. Petersen MC, Shulman GI. Mechanisms of Insulin Action and Insulin
Resistance. Physiol Rev. 2018;98:2133-2223.
8. Ceriello A. The possible role of postprandial hyperglycaemia in
the pathogenesis of diabetic complications. Diabetologia. 2003;46
Suppl 1:M9-16.
9. Bahendeka S, Kaushik R, Swai AB, et al. EADSG Guidelines: Insulin Storage and Optimisation of Injection Technique in Diabetes Management. Diabetes Ther. 2019;10:341-366.
10. Russell-Jones D, Khan R. Insulin-associated weight gain in
diabetes--causes, effects and coping strategies. Diabetes Obes Metab.
2007;9:799-812.
11. Diabetes UK. Insulin and Diabetes. Available at: https://www.diabetes.org.uk/about-diabetes/looking-after-diabetes/treatments/insulin Last accessed: October 2024.
12. Spollett G, Edelman SV, Mehner P, et al. Improvement of Insulin
Injection Technique: Examination of Current Issues and
Recommendations. Diabetes Educ. 2016;42:379-394.
13. Nakhleh A, Shehadeh N. Hypoglycemia in diabetes: An update on
pathophysiology, treatment, and prevention. World J Diabetes.
2021;12:2036-2049.
14. Lowe RN, Williams B, Claus LW. Diabetes: how to manage patients
experiencing hypoglycaemia. Drugs Context. 2022;11.